AFM: Self-healing silk fibroin hydrogel for bone regeneration: dynamic metal ligand self-assembly method
one. Article overview
Although progress has been made in the development of silk fibroin (SF) hydrogels, the current methods for SF gelation have obvious limitations, such as lack of reversible crosslinking, use of non-physiological conditions, and difficulty in controlling the gelation time. In this research, a method based on dynamic metal ligand coordination chemistry was developed to assemble SF hydrogels by the combination of SF microfibers (mSF) and polysaccharide binders. The prepared SF hydrogel exhibits shear thinning and self-healing characteristics, so that it can fill irregular-shaped tissue defects without gel fragmentation. The biomineralization method is used to generate calcium phosphate-coated mSF, which is chelated by the bisphosphonate ligand of the binder to achieve reversible crosslinking. In addition, through the photopolymerization of the acrylamide group of the adhesive, a strong double cross-linked (DC) hydrogel can be obtained, which can achieve in vitro stem cell proliferation and accelerate the criticality of the skull without providing any additional morphogenetic factors. Bone regeneration of size defects. In summary, the self-repairing and photopolymerizable SF hydrogel developed in this research has the advantages of injectability and suitable for shape molding, and has great potential in bone regeneration applications.
Two, graphic guide
Although progress has been made in the development of silk fibroin (SF) hydrogels, the current methods for SF gelation have obvious limitations, such as lack of reversible crosslinking, use of non-physiological conditions, and difficulty in controlling the gelation time. In this research, a method based on dynamic metal ligand coordination chemistry was developed to assemble SF hydrogels by the combination of SF microfibers (mSF) and polysaccharide binders. The prepared SF hydrogel exhibits shear thinning and self-healing characteristics, so that it can fill irregular-shaped tissue defects without gel fragmentation. The biomineralization method is used to generate calcium phosphate-coated mSF, which is chelated by the bisphosphonate ligand of the binder to achieve reversible crosslinking. In addition, through the photopolymerization of the acrylamide group of the adhesive, a strong double cross-linked (DC) hydrogel can be obtained, which can achieve in vitro stem cell proliferation and accelerate the criticality of the skull without providing any additional morphogenetic factors. Bone regeneration of size defects. In summary, the self-repairing and photopolymerizable SF hydrogel developed in this research has the advantages of injectability and suitable for shape molding, and has great potential in bone regeneration applications.
Two, graphic guide
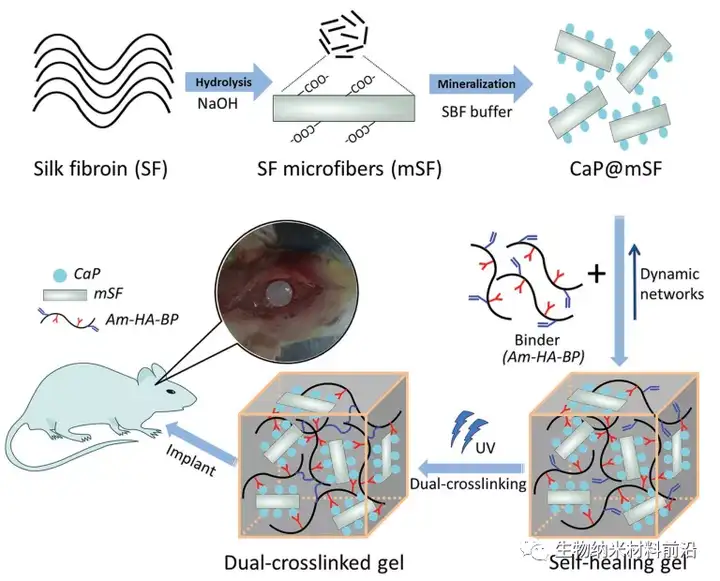
Figure 1. Schematic diagram of the preparation of self-healing SF-based hydrogel for bone regeneration.
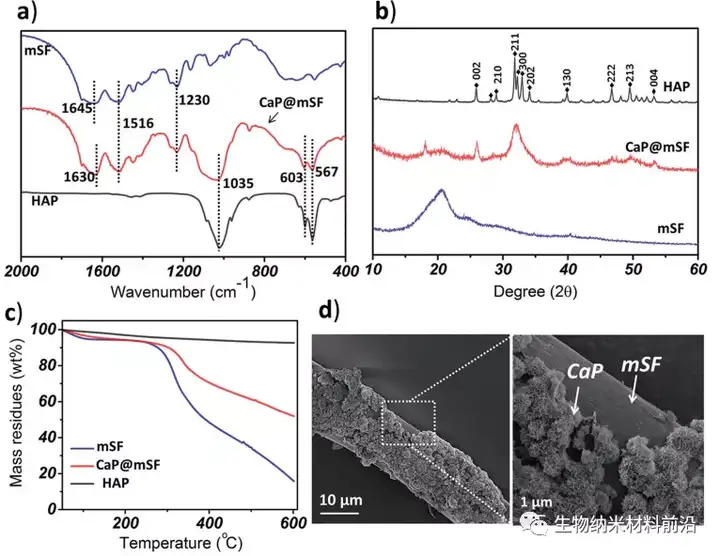
Figure 2. The characterization of CaP@mSF; a) FTIR analysis, b) XRD analysis, c) TGA curve of CaP@mSF.
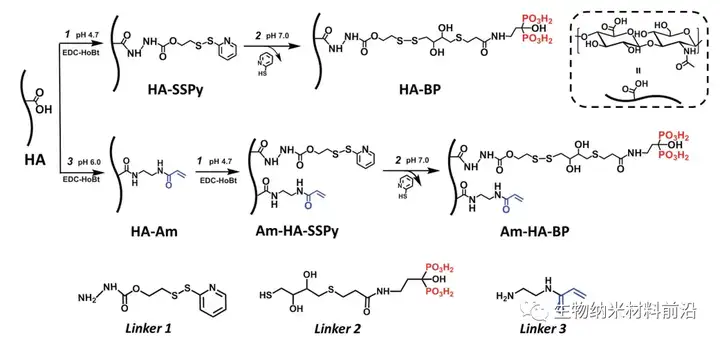
Figure 3. Synthesis of a biopolymer adhesive based on hyaluronic acid (HA).
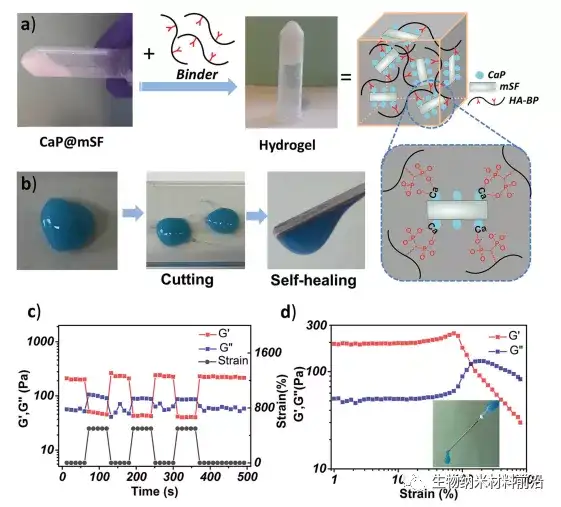
Figure 4. Preparation of HA-BP·CaP@mSF hydrogel and its self-healing properties; a) CaP@mSF dispersion and SF-based hydrogel images; b) Hydrogel is cut into fragments and the cut fragments are connected Images together; c) the storage modulus of the hydrogel under alternating shear strain deformation; d) the transformation from gel to liquid during shear strain.
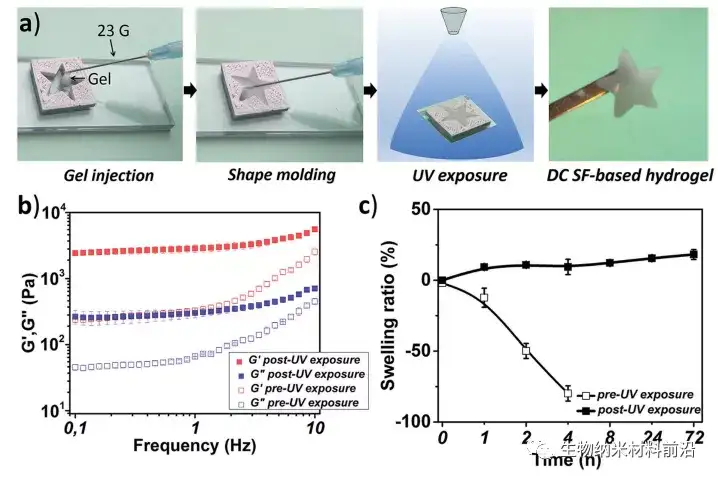
Figure 5 a) Am-HA-BP·CaP@mSF hydrogel formed in a five-star mold; b) Comparison of the mechanical properties of Am-HA-BP·CaP@mSF hydrogel before and after secondary light crosslinking; c) Swelling of SF-based hydrogels before and after photocrosslinking.
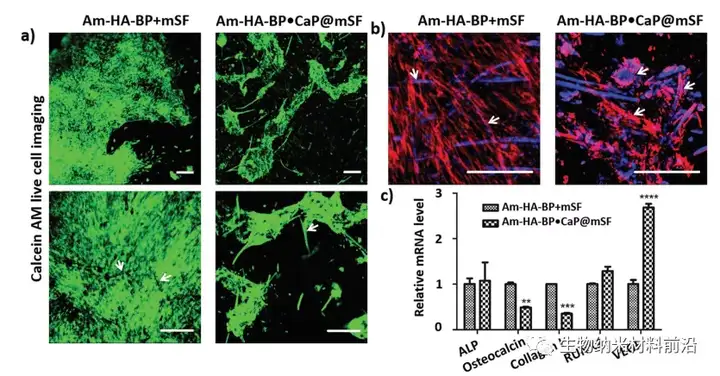
Figure 6. DC Am-HA-BP·CaP@mSF and Am-HA-BP+mSF hydrogel surface hMSCs morphology and related osteogenic gene expression; a) Live cell imaging with Calcein AM on the 14th day; b) Cells were fluorescently stained with cyclic peptide-TRITC (red) and Hoechst (blue) on the 14th day; c) The osteogenic markers of hMSCs on the hydrogel and the relative gene expression of the growth factor VEGF on the 14th day .
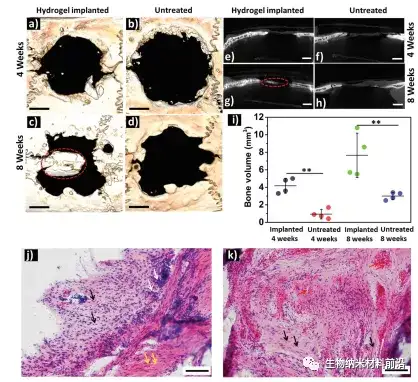
Figure 7. New bone formation after implantation of DC AM-HA-BP·CaP@mSF hydrogel into a rat model of severe skull defect.
3. Full text summary
In this study, the in-situ assembly of SF hydrogels with shear thinning and self-healing properties was achieved through the coordination chemistry of state metal ligands. In order to complete the modular assembly of SF hydrogels, this study used a "top-down" method to prepare mSF with a length of 200 μm and a diameter of 10 μm, and was coated with CaP particles under mild biomineralization conditions. CaP@mSF was produced. These mineralized mSF are combined with bisphosphonate-modified HA-BP to be immobilized in the hybrid hydrogel network. Due to the coordination interaction between the BP group on the adhesive and the Ca2+ ions on the surface of CaP@mSF, HA-BP acts as a natural polymer adhesive for CaP@mSF. The reversible properties of these interactions endow the resulting hybrid hydrogel with shear thinning and self-healing properties. This condition allows the material to be shaped without shifting from the intended implantation site and damaging the hydrogel during injection. In addition, this study designed a HA adhesive (namely Am-HA-BP) with dual functionalization of BP and polymerizable acrylamide (Am) groups, and combined the corresponding Am-HA-BP·CaP@mSF composite material After molding, it is exposed to ultraviolet rays to form a DC Am-HA-BP·CaP@mSF hydrogel, which has a ten-fold enhanced storage modulus. Implanting DC Am-HA-BP·CaP@mSF hydrogel into the skull defect of rats can induce bone regeneration in vivo without adding any growth factors. These findings mean that the developed self-healing and photopolymerizable SF-based hydrogel is a promising injectable scaffold for bone regeneration that can fill irregular-shaped bone defects.
Article link:
DOI: 10.1002/adfm.20170059
DOI: 10.1002/adfm.20170059
This information is sourced from the Internet for academic exchanges only. If there is any infringement, please contact us to delete it immediately.
+86-18915413828(WhatsApp&WeChat)
Previous: ACS Appl. Bio Mater.: